Origin and Background of AIDS
 AIDS (Acquired Immune Deficiency Syndrome) is an infectious disease caused by infections with the Human Immunodeficiency Virus (HIV).
AIDS (Acquired Immune Deficiency Syndrome) is an infectious disease caused by infections with the Human Immunodeficiency Virus (HIV).Origins of AIDS
• 1983 – 1984 French and American scientists isolated the virus from the blood.
• 1999 – Scientists announced that HIV is most likely derived from a kind of chimpanzee. Scientists found a virus, Simian Immunodeficiency Virus (SIVcpz), which has implications on the Apes, and it is very similar to the structure of several subspecies of HIV.
• There are two types of HIV: HIV-1 and HIV-2.
• The origin of HIV-1 is possibly from the African Ape: Chimpanzee.
• HIV-2 is from African monkey: Mangabey.
• In most countries, the HIV infection is caused by HIV-1. Without proper treatment after HIV-1 is infected, more than 90 % of persons will become the HIV-infected patients in 10-12 years.
• HIV-2 mainly distributed in West Africa and in some parts of India, the onset process is relatively slow.
Global Overview of AIDS
• According to the worldwide HIV infection statistics announced by UNAIDS (United Nations Programme on HIV and AIDS) in 2016, the estimated number of worldwide HIV-infected adults and children were around 36.7 million at the end of 2015. In 2015 only, the estimated worldwide new HIV infections were 2.1 million and the number of deaths due to AIDS was estimated to be 1.1 million.
• On the global distribution, the situation is most serious in eastern and southern Africa. In 2015, approximately 470,000 local people died of AIDS, followed by western and central Africa, the estimated number of deaths due to AIDS were 330,000.
• In China, the epidemic of AIDS is generally low, however in some areas and specific population, the infection rates is higher. There is a total of 577,000 people diagnosed with HIV/AIDS surviving at the end of 2015, and it is estimated that 32.1% of those who are infected have not been diagnosed.
• Hong Kong’s AIDS infection rate is relatively low, but new HIV infections are still occurring. An average of about 2 people are diagnosed with HIV every day in 2016.
HIV/AIDS in Hong Kong
• According to WHO standards, infection rate of HIV/AIDS in Hong Kong is currently at a low level.
• On average, about 2 people are diagnosed with HIV every day in 2016.
• The annual infection rate of HIV has reached a historical high in 2015 and 2016.
• Several years ago, specialists from the Department of Health has already pointed out that the HIV/AIDS infection level in Hong Kong is “living on the edge”.
• The promotion of HIV/AIDS prevention education is crucial, aiming to allow every person to understand that HIV/AIDS is a contagious disease that is preventable and treatable. If the general public, including persons infected with HIV, industriously carry out universal preventive measures, and if infected persons persist in receiving medical treatment to maintain the virus level at an “undetectable” level, a decrease in the number of new infections is expected to follow. We believe that these effective measures can prevent the spread of HIV virus.
The Disability Discrimination Ordinance (DDO)
• In Hong Kong, one’s medical history belongs to private information.
• As such, it is not mandatory for a person to disclose his or her medical history to the school or employer; it is also not the usual practice for the government to disclose the medical history of any citizen to his or her school and employer.
• Any person infected by HIV is protected under the DDO.
• As mentioned in the DDO, the definition of disability includes the presence of organisms in the body that cause or are capable of causing disease or illness. HIV infection falls under this definition.
• The right of persons with HIV/AIDS to receive medical treatment is also protected.
• These protections also extend to associates of the infected person. It is unlawful for the associates to be discriminated against, harassed or vilified on the ground of disability of the infected person (an associate includes a spouse, cohabitant, relative, career and a business, sporting or recreational associate).
Problems faced by people with HIV/AIDS
HIV infected people needed to face the problem “how” to disclose their infection to others. Most of them will consider telling the truth to their partners, relatives, health care workers or social workers. Respect and acceptance of communities, with enhance of various support from medical professionals, social workers and peers will benefit for HIV infected people to disclose. Correctly reveal the status of HIV infection will reduce the stress of PLHIVs who are suffering from concealing the disease. It may encourage their partner to receive HIV testing. It also helps those relatives and friends’ to release their doubts and worries about living with HIV-infected day by day.
Although, there is no way to cure HIV infection, those infected people need to take a lifetime medication. Today’s global HIV/AIDS management programs focus on enhance HIV testing, enhance treatment to those HIV-infected, and people with treatment can have successfully HIV inhibited. This will not only reduce the mortality and morbidity of infected people, but also make the infected person had a normal life. In addition, early and effective HIV treatment for those HIV-infected can greatly reduce the HIV epidemic. Anti-retroviral therapy (ART) has been shown to be able to reduce the chance of HIV transmission in sero-discordant couples (where one partner is HIV negative and the other is HIV positive) by up to 96% through suppressing the viral load (the number of virus in human blood) of the HIV positive partner to a low or undetectable level.
On the other hand, infected people needed to coordinate or reorganize their lifestyle to start early lifelong treatment and maintain a stable medication adherence. Those community organizations which provide counseling to support infected people to handle their living styles that affect treatment, enhance compliance with long-term treatment, and persistent surveillance of medication are very important to those infected people and their partner or family, especially for those men and women who plan of establishment of intimate relationships, family and have children.
HIV/AIDS infected people also need to face other health problems that are more common among people living with HIV, including premature aging, cardiovascular disease, chronic liver, kidney disease, cancer and mental health problems. Research showed that rates of depression in PLHIV are as high as 60% vs about 5% to 10% of the general population. Women with HIV are twice as likely as men to be depressed. Therefore, the infected people need to actively maintain mental health to combat or prevent of depression. HIV/AIDS is still a stigmatizing disease globally and in Hong Kong. Infected people have faced embarrassing experiences. Therefore, communities must raise their sensitivity to the needs of PLHIV, the general public should also be appealed for an accepting attitude for PLHIV and populations who are at risk of HIV infection, and infected people are encouraged and empowered to engage in strategy development and its implementation. Working together will make a supportive environment conducive to HIV prevention and care.
Back to section
HIV Prevention

Prevention of transmission and blood contact
Since 1980s, it has been found that HIV transmission rate through blood and blood products transfusion is as high as 90% or more. Developed countries or regions have strengthened the HIV screening testing of blood and blood products since then. Requiring hospitals to provide safe blood and blood products, and to carry out blood and blood products transfusion with careful mind, especially in developing countries or regions, are the prevention methods of HIV.
Other blood-borne transmission of HIV usually occurs via sharing of needles or syringes by injecting drug users, or sharing contaminated tools or personal items with others. Suitable precautions include:
• Encourage injecting drug users to join the methadone treatment programme, the maintenance or detoxification programme; receive drug treatment and rehabilitation services; stop sharing syringe and needle; or use disinfected syringe and needle.
• Requires hospitals, gynecology and dentistry clinics, and beauty clinics to provide proper disinfected tools.
• Fully understand the sterile procedures provided by piercing or tattoo shops.
• Do not share personal items such as toothbrushes, razors or nail clippers.
• Take protective measures to avoid direct contact with blood; wear gloves before handling any wounds. Wounds should be disinfected and covered with dressings.
Prevention of Mother-to-child transmission
The risk of Mother-to-child transmission of HIV is from 15% to 40%. Since preventive programmes were carried out globally with interventions of universal antenatal HIV testing of pregnant women, the infected mother receive antiretroviral regimen during pregnancy till delivery, and after birth, the newborn baby also take a course of antiretroviral therapy, the risk of Mother to child transmission would drop gradually. Please refer to “Prevention of Mother-to-child transmission“ for related prevention measures.
Prevention of transmission through sexual contact
According to the global surveillance record, sexual contact is the main route of HIV transmission. All sexual behavior, poses a certain risk for sexually transmitted diseases and HIV. Individuals should take protective measures and practice safer sex to reduce the chances of sexually transmitted diseases and HIV.
A B C D The principle of safer sex
A = Abstinence: Abstinence or delay the onset of sexual activity
B = Be faithful: Keep the number of specific or restricted partners
C = Use a Condom:Persistence and proper use of condoms and lubricants
D = Drug and alcohol free:No use of dangerous drugs and alcohol
The decision of practice safer sex is an ongoing process and is not easy. According to the data of UNAIDS, it is estimated that when condoms are used consistently, their efficacy in preventing sexually transmitted diseases and HIV is 80% to 85%.
Steps for correct use of male condom
 1. Use a new, good quality latex condom and check the expiry date before use. |
 2. Put the condom on before the penis touches the vagina, mouth or anus. |
 3. With care, hold the condom by the tip to squeeze out the air. This allows room for the semen. |
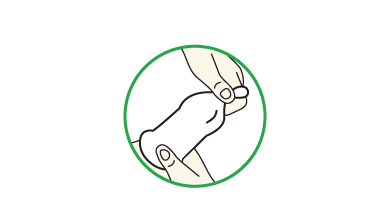 4. Put the condom at the end of the erect penis. Unroll it onto the erect penis all the way down to the hair. |
 5. Use water-based lubricants. Oil-based lubricants can cause the condom to break. |
 6. After ejaculation and before the penis gets soft, grip the rim of the condom and carefully withdraw. |
 7. Gently pull the condom off the penis, making sure that semen doesn’t spill out. |
 8. Wrap the condom in a tissue and throw it in the trash. |
Steps for correct use of female condom
 1. Use a new, good quality condom and check the expiry date every time before use. |
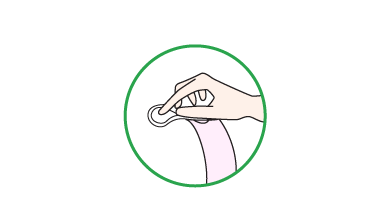 2. Identify the inner ring located at the closed end of the female condom. Use the thumb, the index finger and the middle finger to squeeze the lower part of the condom. |
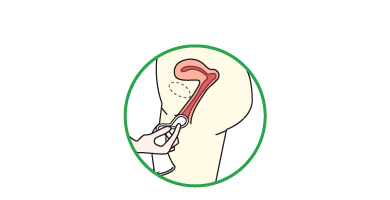 3. Insert the inner ring into the vagina. |
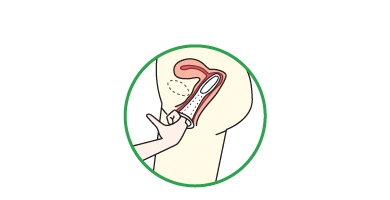 4. Put a finger inside the female condom to push the inner ring further inside the vagina.The outer ring would be left outside of the vagina. |
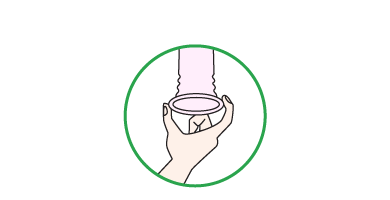 5. After intercourse, twist the outer ring two to three rounds before pulling out the condom to avoid spillage of the semen. |
Other alternatives of prevention of HIV
(A) HIV prophylaxis - Antiretrovirals (ARVs)
HIV prophylaxis: Use ARVs to protect people from HIV infection. There are two types of HIV prophylaxis, Post-Exposure Prophylaxis (PEP) and Pre-Exposure Prophylaxis (PrEP).
1. Post-Exposure Prophylaxis (PEP)
Since 1988, ARVs have been prescribed to block the establishment of HIV infection in an individual, primarily for healthcare workers who had been exposed to the virus. There are two types of PEP - Occupational Exposure Prophylaxis (oPEP) and Non-occupational Exposure Prophylaxis (nPEP).
(a) Occupational exposure prophylaxis, oPEP
Healthcare professionals in hospitals or other clinical services may expose to HIV during work by needle stick injuries or other ways in contact with blood from individuals who are known or at high risk of HIV infection. Research indicates that the average risks of HIV transmission after percutaneous and mucocutaneous exposure to HIV-infected blood were estimated to be 0.3% and 0.09% respectively. Findings from animal studies suggested that ARVs would not be effective if begun more than 72 hours after exposure. Therefore it should be initiated as soon as possible, preferably within 1-2 hours of exposure, and continued for 4 weeks. According to the World Health Organization (WHO), adherence to a full 28-day course of ARVs is critical to the effectiveness of the intervention. A 1997 study of healthcare workers from France, Italy, the UK, and the US came to the conclusion that PEP reduced the risk of becoming infected with HIV by 81% (with a confidence interval of 48-94%).
(b) Non-occupational exposure prophylaxis, nPEP
Non-occupational exposure prophylaxis refers to the use of ARVs after exposure unrelated to work such as mother-to-child transmission or unsafe sex. Administering ARVs to HIV-positive pregnant women and their newborns significantly reduces the risk of HIV transmission during pregnancy, labor, delivery, and breastfeeding. In one retrospective study, initiating zidovudine within 48 hours of birth was apparently able to reduce the transmission risk from 26.6% to 9.3%. For exposure prophylaxis after unsafe sex, experiment showed that because of the differences in duration and amount in contact with body fluids, nPEP could only reduce the risk of HIV infection in emergency situation. nPEP should never be considered as replacement of use of condom to prevent HIV by sexual contact.
2. Pre-Exposure Prophylaxis (PrEP)
It is a new measure to prevent HIV. Pre-exposure prophylaxis is the use of ARVs on high-risk HIV-negative individuals to reduce their risk of HIV infection. Several overseas trials have found that the effectiveness of pre-exposure prophylaxis with antiviral agent to prevent HIV infection in uninfected people ranged from 44% to 86%. Data of CDC, Divisions of HIV/AIDS Prevention showed that daily PrEP reduces the risk of getting HIV through sex by more than 90%. Among injection drug users, it reduces the risk by more than 70%.
PrEP has brought significant effect of HIV pandemic after practicing in US, UK, Australia, etc. In Asia, only Thailand and Taiwan are promoting PrEP. At this stage, only the use of the combination pill Truvada as PrEP on high-risk individuals was studied. Truvada is the combination pill containing tenofovir (Viread) and emtricitabine (Emtriva). People on PrEP are recommended to monitor the following items every 2-3 months: HIV and STIs screening, medication adherence and side effects of PrEP according to the guideline of Centers for Disease Control and Prevention (CDC). Truvada should only be prescribed by registered medical practitioners. Therefore, individuals at high risk of HIV infection considering PrEP are advised to discuss his/her health condition with a registered medical practitioners in a medical setting.
It is important to note that either PEP or PrEP is additional preventive measures, rather than a ‘cure’ for HIV. Neither PEP nor PrEP are 100% effective. Risk of getting HIV from sex can be even lower if combine PrEP with condom users and other prevention methods.
(B) HIV treatment as prevention (TasP)
Public health practitioners and prevention advocates emphasize that HIV treatment is an effective preventative approach for HIV and important factor in controlling the HIV epidemic. When the infected person receives anti-retroviral therapy (ART) and successfully controls the amount of virus, it is possible to reduce the amount of virus in the blood, semen, vaginal and rectal secretions to a very low level (or undetectable), thereby reducing the chance of transmission. In 2011, a study showed that ART is able to reduce the chance of HIV transmission in sero-discordant couples (where one partner is HIV negative and the other is HIV positive) by up to 96% through suppressing the viral load (the number of virus in human blood) of the HIV positive partner to a low or undetectable level. UNAIDS and the WHO have officially announced in 2015 that 90-90-90 as treatment target to help end the HIV/ AIDS pandemic by 2020. If these three objectives are successfully achieved, the number of new infections will be reduced to 500,000 per year. 90-90-90 by 2020 means that 90% of People Living with HIV (PLHIV) are diagnosed ,90% who know they are HIV positive are receiving treatment and 90% who are on HIV treatment have suppressed viral load. Public health practitioners and prevention advocates are actively promoting effective interventions and hope to meet the new goals of the UNAIDS.
Back to section
HIV Testing

Most HIV infected persons have no specific or obvious signs or symptoms. It is impossible to tell if a person has the virus just by looking at, or talking to, him or her. A person has HIV can pass the virus to others even if he or she is asymptomatic. The only way to know if someone has HIV is by an HIV antibody test.
Antibodies are usually produced by the body when it is exposed to an infection. Antibodies are one of the body’s tools for fighting infections. The antibodies against HIV, however, are not protective in nature. HIV antibody testing is a blood test carried out to find out if one has contracted HIV.
As it takes up to 3 months for a detectable quantity of HIV antibodies to be produced, the infected person can transmit the virus even though an HIV antibody test shows a negative result during this period, so called Window Period. It is the time between initial infection with HIV and when a positive test result occurs.
You should consider getting tested if you or your sexual partner have ever had unprotected sex, sexually transmitted infections, and/or shared needles or syringes to inject drugs. Please call the AIDS Hotline at 2780 2211 for free and anonymous HIV antibody testing services.
Back to section
Mother-to-child transmission

HIV may cause placental infection and subsequently intrauterine infection of fetus. This possibility is supported by the findings that some placental cells express CD4, and the fact that two peaks of HIV positivity can be detected in the infected neonate: Around 40% of the HIV infected infants turned into AIDS patients within 3 years.
Without interventions, the risk of Mother-to-child Transmission (MTCT) varies between 15-40%, depending on factors such as breastfeeding, maternal plasma viral load, clinical status, and the antenatal CD4 T-lymphocyte counts. The maternal plasma viral load is recognized as the strongest predictor of transmission. The use of antiretrovirals and HAART during weeks 14 to 34 of pregnancy can significantly reduce the viral load and thus the risk of MTCT. A combination of interventions (including combination antiretroviral therapy, caesarean section and avoidance of breastfeeding) is associated with a vertical transmission rate of less than 1-2%.
To address the problem of missed diagnosis, From September 2001, all antenatal patients booked in public antenatal clinics (Hospital Authority hospitals and Maternal & Child Health Clinics) are offered free HIV antibody test on top of their usual antenatal blood tests. Prompt diagnosis and intervention is the key to effective MTCT prevention.
MTCT is unique in the sense that a window of opportunity exists whereby appropriate biomedical intervention can prevent the occurrence of the infection. Furthermore, as HIV infected women are enjoying better general health while receiving highly active antiretroviral therapy (HAART), they may be more willing to start a family and rear a child, whereas in the past most would avoid or terminate pregnancy.
Back to section
Opportunistic Infections

HIV Disease Progression
• The time it takes from infection of HIV to diagnosis can range from a few months to about 10 years
• HIV primarily attack and destroy a white blood cell called CD4 or T-lymphocytes. This causes the human body to gradually lose its natural immunity to withstand infections and cancers; which usually holds no threat to a person with an intact immune system.
• CD4 cells are a part of the immune system and it protects the body by fighting off infections when the body is attack by “intruders” such as viruses and bacteria.
• Acute infection stage is referred to the initial stage of HIV infection, where large amount of virus are being produced in the body using CD4 cells in this process; hence CD4 count can fall rapidly. During this phase, viral load in the blood can reach 106 copies/ml.
• The normal range of CD4 cell count is around 500-1500 cell /mm3. When CD4 drops to below 200 cell /mm3 or CD4 is less than 14% of all lymphocytes. The immune system is now weak and it is vulnerable to other illnesses.
• As the HIV infected person’s immune system deteriorates and cannot fight of opportunistic infections and cancers, this person is regarded as having acquired immunodeficiency syndrome (AIDS).
• If adults infected with HIV do not receive correct drug treatment, about 50% will present AIDS within 10 years.
• If children infected with HIV do not receive correct drug treatment, about 40% will present AIDS within 3 years.
• If CD4 count remains in 50-200 cell/mm3, it is likely that within 18-24 months AIDS patient will develop opportunistic infections and the likelihood of dying is 50-70%.
Opportunistic Infections
HIV primarily destroys CD4 cells/T lymphocytes and causing natural immunity to decrease till it cannot fight off different infections and cancers, that are usually not threats to a person with a good immune system. These infections are called “opportunistic infections”. There are currently twenty six illnesses used to diagnose AIDS on the HIV surveillance system in Hong Kong. When a person living with HIV suffers from any one of these illnesses they will be classed as AIDS patients. The most common three illnesses for AIDS diagnosis in Hong Kong are: Pneumocystis carinii pneumonia (PCP), tuberculosis (TB) and fungal infections.
Common Opportunistic infections that affects:
• Respiratory tract: PCP , TB can cause difficulty in breathing
• Central Nervous system: Toxoplasmosis and cryptococcal meningitis that affects the nervous system
• Opthamic: Cytomegalovirus retinitis can cause blindness.
• Gastrointestinal: Cytomegalovirus gastroenteritis/ colitis, cryptosporidiosis can cause bloody stool and ulceration of the esophagus.
• Skin: Herpes simplex (cold sores, genital herpes ), herpes zoster (chicken pox) and molluscum contagiosum.
• Affecting Mycobacterium Avium Intracellulare (MAI), Penicillium Marneffei of the body, possibility of fever, anemia, Hepatosplenomegaly etc.
• Mouth and throat: Candidiasis (fungal infection) causes white spots, ulcers and swallowing difficulties.
Back to section
Treatment for HIV/AIDS

Currently HIV cannot be eradicated from human bodies, but medical treatment is possible for complications or diseases developed because of AIDS, e.g. opportunistic infections. Many drugs against AIDS are available, and Highly Active Anti-retroviral Therapy (HAART, or “cocktail therapy”) has been developed. It can suppress replication of virus inside human bodies, effectively reducing the viral load to an undetectable level and hence minimizing the damages done to immune system.
AIDS treatment can be categorized into two parts:
• Drug treatment to suppress replication of virus, stabilizing patients’ conditions
• Prevention and treatment for opportunistic infections due to weakened immune system
Adopting the above two treatments simultaneously can strengthen patients’ health, improve quality of life and prolong life expectancy. Regular follow-up consultations with doctors will help monitoring conditions of PLHIV, providing early diagnosis and treatment of complications.
Although HIV/AIDS cannot be eradicated, current treatment in Hong Kong has significantly reduce disease incidence and mortality rate. The time of incidence is also pushed back for about 50 years. Caring for PLHIV is similar to caring for chronically ill patients. AIDS treatment in Hong Kong is primarily provided by Department of Health at Kowloon Bay Integrated Treatment Centre and public hospitals under Hospital Authority. Clinical services are provided to PLHIV in need. Currently, about 60% PLHIV receive direct treatment and care services from Kowloon Bay Integrated Treatment Centre.
Cocktail Therapy
• Dr. David Ho first introduced the concept of “cocktail therapy”, possibly the most influential development in the treatment towards HIV/AIDS.
• "Cocktail therapy", as known as HAART, is a combination of at least three antiretroviral drugs. Maintaining medication adherence above 95% for a long period of time can effectively suppress the HIV viral load in the blood to "undetectable levels".
• "Undetectable levels" in viral load means that the amount of HIV in the sample of blood of an HIV-positive person decreases to a level that cannot be detected by standard viral load tests. Though the viral load can reach a very low level, the HIV remains inside the body.
• Therefore, while an HIV-positive person under HAART got viral load under detectable levels, to protect oneself and others, some general preventive measures should still be taken to avoid HIV transmissions through sex, blood, giving birth and breastfeeding. By doing so, an HIV-positive person can prevent himself/herself being infected with other HIV, viruses and bacteria and fend off the chances of undermining the effect of treatment.
• According to researches conducted in Canada, U.S.A. and South Africa, the number of new HIV infections decreases when the amount of HIV-positive people in the community stick to the HAART increases and their viral loads lowered. In addition, the preliminary findings from a clinical research of South Africa shows that successful treatment in HIV-infected people can bring down the number of new infections for over 90%.
The Importance of Regular Medications
• To achieve a successful treatment, an HIV-positive person/ an AIDS patient must strictly follow the rules on medications and adhere to treatment plans in order to lower the possibility of drug resistance and treatment failures. Otherwise, the HIV inside the body could eventually become drug resistant and thus compromising the treatments.
• Drug resistance means that the ability of medicines containing the replication of HIV is reduced. It is caused by the mutation of the virus when it seems to adapt to the drugs and alter its way of attaching to immunal cells and multiplying. Forgetting to take medications or a temporary pause on medications provides chances for HIV to mutate and reproduce.
Common side effects of antiviral drugs
• Every type of drug has potential side effects. While an antiviral drug may be an effective treatment for patients with HIV/AIDS, it may also bring toxic reactions and side effects.
• Common side effects usually last several weeks upon commencement of the treatment. The situation usually improves when the body gradually adapts to the drug. Medical professionals provide patients with pre-medication counselling which includes dealing with side effects, in which patients should not stop the medication or alter the dosage even if they experience discomfort after taking the medication. Also, patients are provided with channels to discuss with medical professionals on ways to alleviate the side effects, such as coordinating with the diet and adjusting the time of medication intake. If the side effects persist or worsen, the medication plan should be reviewed at an appointment with the doctor.
Temporary side effects include:
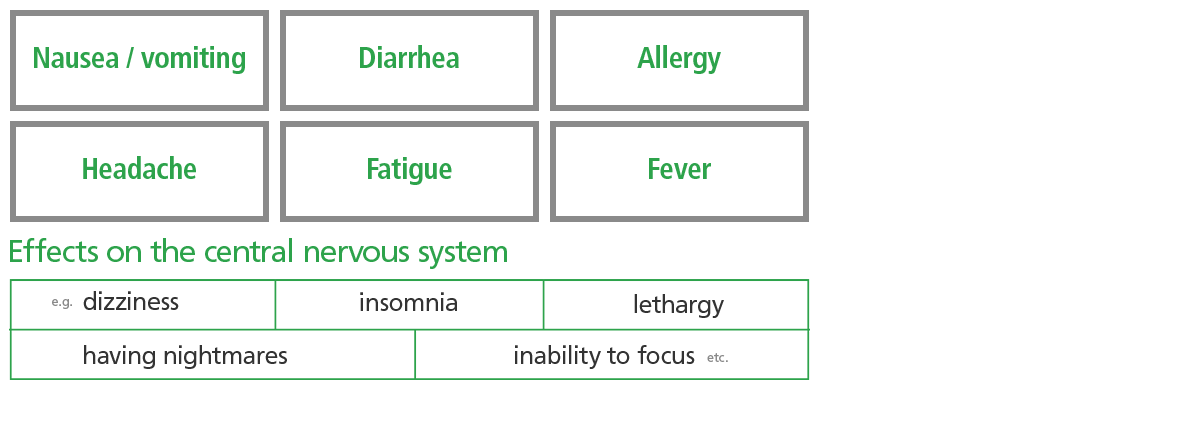 |
Possible chronic side effects include:
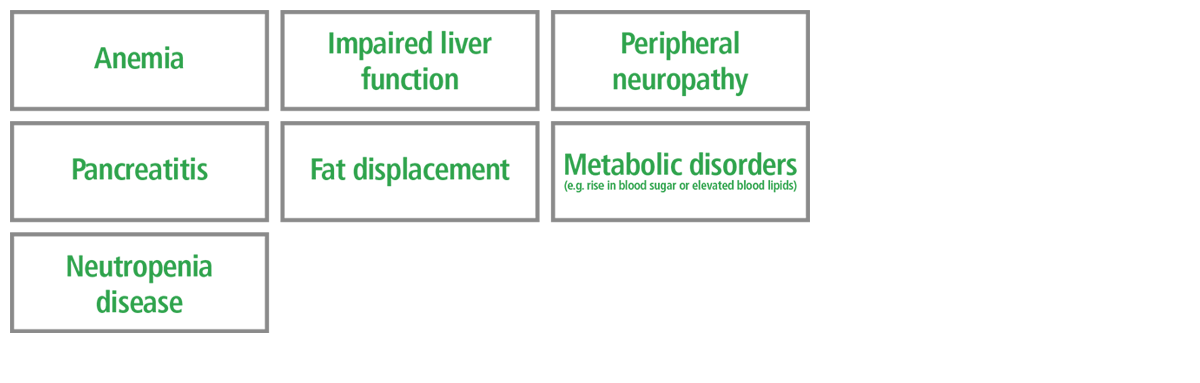 |
Back to section
AIDS in Hong Kong

1984
The first case of HIV infection in Hong Kong was diagnosed. An HIV/AIDS surveillance system started to develop within the Medical and Health Department. And between Dec 1984 and Dec 1994, 63 patients were detected to be HIV positive, out of a total of 231 haemophiliacs screened in Hong Kong. Infection could be traced back to before August 1985, when safer heat-treated clotting factors were not yet available. Psychosocial impacts were obvious in this group of patients because of the double blow of HIV infection and haemophilia. Amongst the more evident problems were obstacles in schooling, employment difficulties, and disturbed relationships with family and friends, to mention a few. 11 patients (17.5%) were known to have progressed to AIDS. Medical treatment, psychosocial support and financial assistance are integral components of an effective AIDS care program for them.
1985
The first case of AIDS in Hong Kong was reported. HIV clinic has been set up by the Government. Commencement of AIDS counselling and HIV antibody testing service by the Government. On the other hand, The Hong Kong Red Cross Blood Transfusion Service commenced screening of all donor blood. And safer heat-treated blood product was produced by the Government to replace unsafe products used in the treatment of haemophilia.
1986
3 patients were reported to have contracted HIV through transfusion of contaminated blood in Hong Kong.
1987
Sexual contact has become the main route of transmission for new infections. The cumulative total number of HIV infected persons reported as of the end of the year was 107. And the AZT (zidovudine) treatment was first introduced to patients with AIDS.
1988
AIDS Counselling and Health Education Service were expanded, with the introduction of a hotline for the public (2780 2211). The first ‘World AIDS Day’ was commemorated on 1 Dec, parallel with education activities for various community groups. And the Consumer Council released its first report on the quality of condoms on sale in Hong Kong and aroused public concern about safer sex.
1989
The first case of HIV infected drug user in Hong Kong was reported.
1990
The Governor appointed the Advisory Council on AIDS. It is a permanent non-statutory body to advice on AIDS policies in Hong Kong. Through fundraising, Hong Kong non-governmental AIDS organizations have been set up and maintained their operations.
1991
A female commercial sex worker was reported to be HIV infected. Female condoms are available in Hong Kong to help women practice safe sex.
1992
The second anti-HIV drug, DDI (dideoxyinosine) became available in Hong Kong. A British dentist, Mike Sinclair is the first AIDS patient who disclosed his condition to the media in Hong Kong. Sinclair’s body is graphically presented in various stages of declining health spanning to his very last days interspersed with interpretive comments by Chinese doctors, nurses and AIDS officials. Even the widely publicized photo of Sinclair with the Governor’s wife serves to reinforce his corporal identity as an isolated suffering body, a symbol of hopelessness.
1993
AIDS Trust Fund was set up by the Government, to provide ex-gratia payment to HIV infected haemophilia, and to support public education and service projects on AIDS. Three sub-committees are set up under the Council to look at the proposals applying for funding from NGO and research bodies. They were Committee on Education and Publicity on AIDS, AIDS Services Development Committee, and the Scientific Committee on AIDS.
1994
First case of mother-to-child transmission of HIV has been reported in Hong Kong. And the cumulative HIV infection reported 520 cases. With the support of Government Council of AIDS Trust Fund and the Keswick Fund, The Society for AIDS Care was established with aim to provide support to people living with HIV/AIDS (PLHIV) as well as their care-givers.
As AIDS was not an illness known to many at the time, HIV was considered as highly infectious and contagious that people will catch the disease without physical contact. Since medication targeting at the virus was still in the early stages of development and only a few drugs were available, those who had AIDS reassembled the announcement of a death sentence. The Society for AIDS Care provided both home care and palliative services to help PLHIV and their care-givers to go through the most difficult time with limited drug therapy. The palliative service provided a lot of relieve to the patients as well as their care-givers to help them going through the last moments of life with respect and dignity. Bereavement counseling was given to care-givers for a period of up to two years.
1995
The Disability Discrimination Ordinance was passed by the Legislative Council and put into practice in next year. Under the Ordinance, PLHIV are protected against discrimination, harassment or vilification in the areas of employment, education, services and facilities, clubs and sporting activities etc. This protection includes their families and associates. Hospitals or Clinics cannot refuse to treat people on the ground of having HIV/AIDS. PLHIV and their families have an equal right to access to welfare services under the same set of eligibility requirement, like any other citizen. PLHIV can perform the inherent requirement of most jobs as far as his or her health condition allows. It is unlawful for the employer to dismiss people with HIV/AIDS on the ground of their HIV status and for colleagues to avoid, harass, or vilify them because of their HIV status.
The Government announced the establishment of an integrated day treatment centre for HIV, sexually transmitted diseases and dermatology patients in Kowloon Bay. The proposal was met with strong objection of residents of nearby.
1996
A 14-year-old girl was reported to have acquired HIV through sex. First protease inhibitor, saquinavir, used in Hong Kong to treat patients with AIDS. The Hong Kong Equal Opportunities Commission, an independent statutory body funded by the Government, was established to eliminate discrimination based on sex, disability and family status.
1997
Report of a probable case of transfusion-related HIV infection in a child. The Red Ribbon Centre (an AIDS education, research and resource centre) was set up by the Department of Health, with a capital supported by the Council for the AIDS Trust Fund.
Hong Kong Advisory Council on AIDS, Lions Clubs International District 303 - Hong Kong & Macau, and The Chinese University of Hong Kong invited Dr. David Ho, MD, Time Magazine’s Man of the Year 1996, to visit Hong Kong. The work of Dr. Ho has led to the development of highly active antiretroviral therapy (HAART), which shifts HIV from a terminal to a chronic illness.
The Hong Kong Scientific Committee on AIDS has published “Procedure for Management of Needlestick Injury or Mucosal Contact with Blood or Body Fluids - General Guidelines for Hepatitis B, C and HIV Prevention” and proposed recommendations for HIV Post-Exposure Prophylaxis, PEP. It suggested after occupational exposure to HIV, those health care workers have to take anti-HIV drugs as chemoprophylaxis at a specific period to reduce the risk of infection. Studies have shown that the risk of HIV infection can be reduced by 81% (with a confidence interval of 48-94%).
1998
The cumulative total number of HIV infected persons reported as of the end of the year was 1,146. The Hong Kong Coalition of AIDS Service Organizations (HKCASO) was formed in February. Its members consist of NGOs which deliver on-going HIV/AIDS programs or have a particular interest in supporting people with HIV/AIDS. HKCASO exists to facilitate communication between its member agencies and to advocate on policy issues relating to HIV/AIDS in Hong Kong.
1999
The Society for AIDS Care has been providing rehabilitation services to PLHIV, assisting PLHIV to keep up their independency and minimize the occurrence of permanent physical damage. The better physical ability they have, the better quality of life they gain. The enhanced physical fitness helps them integrate to community with minimal physical limitation.
2000
The Society for AIDS Care ceased the hospice service and a new Day Center was established. The demand for hospice service for AIDS care declined drastically with the emergence of antiretroviral drugs, which profoundly lengthen the life span of AIDS patients. The day center served to provide peer support service and support for patients in coping with taking the medication. As a pioneer in HIV patient care, The Society for AIDS Care delivered education on HIV care, especially on the aspect of practice of “Universal precaution”, and “Acceptance of HIV patients” to over 3000 nurses within the public and private hospital settings.
Department of Health provides psychiatric services to the PLHIVs, alongside the medical clinic in Integrated Treatment Centre (ITC) at Kowloon Bay.
2001
Mother-to-child transmission is one of the transmission routes of HIV. From Sep, all clients attending the prenatal care in Hospital Authority (HA) hospital or the Department of Health and the Antenatal clinics will be offered the HIV test as part of routine antenatal blood testing. Early detection and treatment has been proven to be effective in reducing the chance of mother-to-child HIV transmission by two-thirds. SAC is the only organization in Hong Kong that complements the successful HIV prevention in Mother-to-child-Transmission.
2002
Nucleic amplification test was introduced for blood donation in Hong Kong Red Cross, which further enhances blood safety.
2003
‘Universal HIV Antibody (Urine) Testing in Methadone Clinics’ were piloted in 3 Methadone Clinics as part of the AIDS prevention efforts by Department of Health. During that period, a total of 2,456 attendees at these three clinics were offered urine testing for HIV antibodies and 1,834 of them performed the test. 9 cases were found positive and referred for appropriate follow-up consultations. ‘Universal HIV Antibody (Urine) Testing in Methadone Clinics’ Programme were rolled out in all Methadone Clinics from 2004.
2004
Pilot study to examine the feasibility and applicability of rapid HIV test in AIDS Counselling and Testing Service in Department of Health.
2005
Council for the AIDS Trust Fund launched an additional ex-gratia payment scheme to provide long term financial assistance to HIV infected haemophilia patients. HIV Medicine and Care Programme is one of the four main core programs of Special Preventive Program, including clinical and community services located in ITC, HIV testing and counselling services via the AIDS Hotline. ITC is the main clinical premises where the Department of Health provides its clinical service, with about 60% of the HIV caseloads are seen in Integrated Treatment Centre while the rest are taken care by the Queen Elizabeth Hospital and Princess Margaret Hospital.
2006
SAC has commenced the HK-China AIDS Training Program, to promote good practice in HIV/AIDS care and prevent work and helps strengthen better collaboration in fighting against HIV/AIDS in Hong Kong and China. One of the focus work province is Henan. Henan is well-known for high prevalence of HIV infection in China due to illegal blood collection in 1990s.
In Feb, the Department of Health announced a cluster of HIV-1 Subtype B Infections was detected. The route of HIV transmission in most of the cases detected in the cluster was unprotected homosexual / bisexual contact. A press meeting was held by Centre for Health Protection (CHP) on the announcement of two clusters of HIV cases being detected in Hong Kong, indicating fast rapid local HIV transmission. In Jul and Oct, a gay man HIV testing hotline and website was launched to provide information on HIV/AIDS, counselling and testing service to men who have sex with men by Department of Health.
2007
HA introduced rapid HIV testing (for delivering mother with unknown HIV status) into the ‘Universal Antenatal Testing Programme’.
2008
SAC organized an annual AIDS Walk to improve public awareness on AIDS, and to raise funds for sustaining our services for PLHIV. Through the walk, it hoped to raise funds for the programs that focus on AIDS prevention, mother-to-child prevention, support and care for HIV/AIDS patients and rehabilitation for those combating AIDS in Hong Kong. By opening the walk to the public and making it a family event, it also hoped to raise awareness of the issue that affects thousands of people in Hong Kong.
2011
According to a clinical trial on patients who could adhere to their medications in early days, early treatment reduced HIV transmission to an uninfected partner by 96%, which can be considered as “extremely low risk”.
2012
A surgeon in the Eastern Hospital confirmed to be HIV+. HA has given priority to 140 patients who have been treated by the doctor over the past two years. A total of 137 people have been successfully contacted, with 130 of them have agreed to undergo HIV testing and all results were negative.
2013
A study conducted by the Accident and Emergency Department (A&E) of Queen Mary Hospital, from 2001 to 2011, the clinical data of 105 AIDS patients admitted to the A&E department, of which 44 of them were diagnosed as "invisible patients", who were admitted and diagnosed with HIV at A&E. Their average age is 41-year-old. 77% are male, mostly heterosexual.
The observed reduction in HIV transmission in a clinical trial setting demonstrates that successful HAART use by the person who is HIV positive is as effective as consistent condom use in limiting viral transmission. For the first time, The British HIV Association and the Department of Health’s Expert Advisory Group on AIDS published a position statement on the use of HIV treatment by PLHIV to reduce the risk of transmission. The document states that the transmission risk during vaginal intercourse will be “extremely low”, provided certain conditions are fulfilled, including (1) there are no sexually transmitted infections in either partner (the document clarifies requirements for STI screening, including following sexual relationships outside a primary partnership); (2) the person with HIV has had a sustained plasma viral load below 50 copies/ml for more than 6 months, including the most recent test; (3) viral load testing occurs every 3 to 4 months. The position statement notes that no single prevention method can completely prevent HIV transmission. Moreover, antiretroviral treatment has no effect on other sexually transmitted infections, whereas condoms can prevent their spread.
2015
CHP found 2 cases of HIV mother-to-child transmission, one of whom was diagnosed at 1 year of age. The mother had antenatal HIV antibody test negative. It does not rule out that she was infected in the late pregnancy and then transmitted to her baby. Dr. KH Wong of CHP had mentioned the need of learning from the United States which suggested second HIV antibody testing for pregnant women at 36 weeks pregnancy.
It has been reported that from 1994 to 2015, 43 health care workers have voluntarily reported cases of HIV infection. HA does not require public hospital staff to report medical records for the protection of privacy. Dr. Pierre Chan, president of the Hong Kong Public Doctors' Association said that if the universal precaution is practiced properly, the risk of HIV transmission is very low.
2016
The Hong Kong AIDS Advisory Council has proposed HIV/AIDS Strategies for coping with the AIDS epidemic in the next five years (2017-2021). It is estimated by that 2021, the number of PLHIV in Hong Kong will increase from 6,500 to 8,800, up to an increase of 35%. The Advisory Board recommends that the use of condoms has to be increased from 60% to 70% or more by 2020 to control the epidemic.
An ENT specialist refused to carry out an operation for a HIV patient. The patient sued the doctor for breaching the Disability Discrimination Ordinance at the District Court. The original prosecution pointed out that universal precaution is the general principle for surgery, based on the assumption that every patient is with infectious disease. A medical professional should not discriminate and label HIV infected, and cannot refuse to provide service to patient on the ground that patient has HIV/AIDS.
2017
Princess Margaret Hospital Medical Consultant Dr. Tsang Tak Yin, Owen stated that "The management of HIV/AIDS will lead to test and treat, AIDS has become a long term disease by terminally ill." The new approach to contain HIV transmission further confirms that with proper treatment and care, PLHIV can work and live like normal people with sustain health and can re-integrate into the community with proper support. Keeping people in HIV care settings such as our Society encourages patients not to fall out from care setting which will definitely increase their chance of drug adherence.
Back to section
Frequently Asked Questions

Q: What is AIDS?
A: AIDS stands for Acquired immunodeficiency Syndrome; it is caused by infection with Human Immunodeficiency Virus (HIV). After invading the body, HIV gradually damages the immune system and destroys white blood cell. Symptoms of HIV infection may not be recognized for 10 years or even longer. Its common transmission means are unprotected sex (both vaginal and anal), sharing of needles, mother-to-baby and unscreened blood transfusions.
Q: What is the difference between HIV+ patients and those with AIDS?
A: An HIV+ patient is one infected with the virus, but hasn’t suffered from opportunistic infections yet.
Q: How prevalent is HIV/AIDS in Hong Kong?
A: According to the figures in 2016, there are more than 170 new cases in each quarter in average, meaning that about 1.9 persons get diagnosed each day. Sexual transmission remained the major mode of HIV transmission.
According to Hospital Authority, there were 725 new cases reported in 2015 and 692 new cases in 2016, bringing the cumulative total of reported HIV infections to 8,410 since 1984.
Q: What is the significance of medication for HIV/AIDS?
A: There is no cure for AIDS, but it can be controlled under active medication. However, if patients do not take the prescribed medicines on time, they would develop drug resistance, minimizing the effectiveness of medication.
Q: How are PLHIV different from others?
A: They bear no physical difference. They can resume normal social interactions. As saliva contains very minimal amount of HIV, sharing food and kissing would not pose a threat of transmitting the virus.
Q: Why do people living with HIV/AIDS (PLHIV) need physiotherapists?
A: PLHIV usually suffer from several physical complications because of immunodeficiency and side effects of the prescribed therapy. After comprehensive physical examination, physiotherapists can help them with rehabilitation to relieve impairments and maximize their recovery, so that they can integrate back into their neighborhood.
Q: Why do PLHIV need help?
A: About 50% of people living with HIV/AIDS also suffered from depression due to stress of the sickness. Many of the patients are afraid of being discriminated and rejected, and hence choose not to disclose their identity, contributing to the stress in addition to physical pain.
Q: How does SAC’s mother-to-child transmission prevention works?
A: HIV+ women in healthy condition can get pregnant and give birth without transmitting the virus through medication, careful monitor and avoidance of breast-feeding. With our prevention program, the rate of the fetus becoming HIV+ can be reduced from 40% to below 2%.
Q: How can I receive more information about HIV/AIDS?
A: You can receive more information about HIV/AIDS by visiting http://www.info.gov.hk/aids/english/link.htm
Back to section


 Origin and Background of AIDS
Origin and Background of AIDS HIV Prevention
HIV Prevention HIV Testing
HIV Testing Mother-to-child transmission
Mother-to-child transmission Opportunistic Infections
Opportunistic Infections Treatment for HIV/AIDS
Treatment for HIV/AIDS AIDS in Hong Kong
AIDS in Hong Kong Frequently Asked Questions
Frequently Asked Questions





